Serological endpoints: Hemolysis
Complement-mediated lysis of red cells can occur following the binding of antibodies to red cell antigens, as per Figure 1 below. Because complement activation requires at least two Fc portions of antibodies to be in close proximity, most hemolysins are IgM isotype, which circulates as a pentamer; very dense binding of IgG is otherwise required to activate the complement cascade.
However, since in most cases agglutination is the preferred end-point in TML testing, samples are usually collected in either EDTA (which inhibits completion of the complement cascade at the point of C1 activation) or heparin, which prevents the cleavage of C4 in the complement cascade. In agglutination-based assays, there may still be sufficient complement activation to lead to C3 deposition on the RBC surface, but not enough to complete the formation of the membrane attack complex and thereby trigger hemolysis.
Only when the complement-activating capacity of an antibody is of interest is it preferred to collect samples in non-anticoagulated tubes. When collected without a calcium binder such as EDTA or citrate, the plasma in the sample tube becomes serum as fibrinogen is cleared through activation of the coagulation cascade.
Figure 1: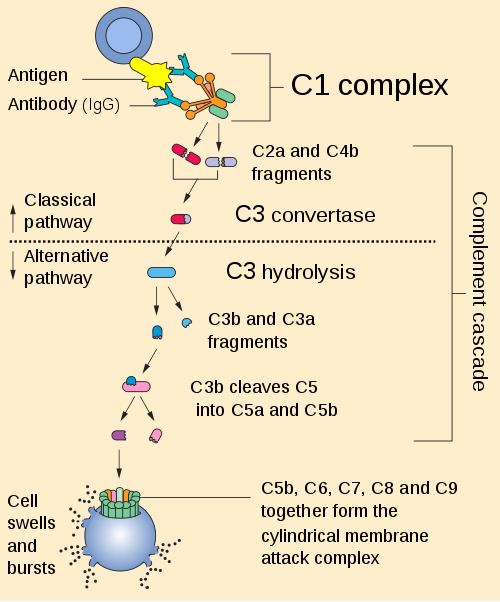
Image from: commons.wikimedia.org
Next page: Serological endpoints: Hemolysis - Additional Notes on Donath-Landsteiner Testing
