Approach to the Antibody Panel:
1: Determine which rows have negative reactions:
These non-reactive rows will be used to perform exclusions. For now, panel cells that showed positive reactions can be ignored
2: Cross off any antigens the non-reactive reagent red cells are homozygous for:
In some centres, ruling out antibodies against specific antigens requires demonstration of non-reactivity with two different homozygous cells. While this provides an additional level of confidence, it often results in a need for a larger number of panel cells to test against. For the purpose of this course, exclusion against a single homozygous cell will be considered sufficient.
Because homozygous K-positive cells are extremely difficult to source due to the high prevalence of the k antigen, exclusion against two K+k+ cells is therefore often considered sufficient.
- Note: because the P antigen is the product of several different genes, its expression is sometimes described as weak vs strong rather than as hemizygous or homozygous; exclusion against any P-positive cell is generally acceptable. The Xga gene carried on the X chromosome, by contrast, can only be homozygously expressed in women. As this antibody is very rarely encountered, however, most panels do not bother to report cell dosage, and this antigen, too can be eliminated with any single cell that is Xga-positive.
3: Once all exclusions are complete, look at the remaining positive reactions. Do they fit a pattern?
Rules for what constitutes a proof of association vary from centre to centre, but a commonly accepted approach is the “rule of three”: if three cells that express the antigen in question all react with the patient’s plasma, and three cells that don’t express the antigen are also all non-reactive, the antibody can be considered to have proven specificity against the antigen in question. See Figure 2 for a completed panel and Table 1 for probability values.
- Note: When assessing for more than one antibody, the same cell cannot be used twice. For example, a cell that expresses the C and the Fya antigen can only be used to prove an association with one or the other antigen, not both.
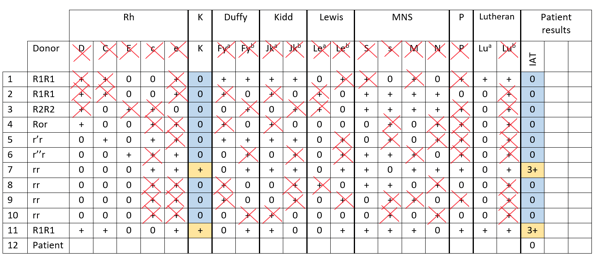
Figure 2: A completed antibody panel that demonstrates anti-K. In this panel, antibodies against all other clinically significant antigens (Rh, Duffy, Kidd, Ss) have been ruled out, in addition to Lewis, MN and P. Exclusion of Lua is not necessary since it is a low-frequency antigen and the pattern of reactivity does not fit.
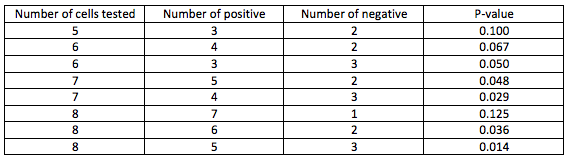
Table 1. Probability value, as calculated by Fisher’s exact test, varies depending on how many positive and negative reactive cells are used to rule in an antibody. For example, in Figure 2, there are 2 positive cells that are reactive for anti-K, and 9 negative cells that are non-reactive for anti-K. Using Fisher’s exact test this computes to a p-value of 0.0045, meaning we can be fairly confident an anti-K is present. (Table adapted from the AABB Technical Manual)
4: Determine if additional cells are required to complete the investigation, either to provide additional evidence of association with an antigen, or to rule out other common, clinically significant antibodies.
Sometimes the cells originally used for the antibody screen are all that is required. Other times, an entire additional panel is required. A skilled serologist can often complete an investigation by carefully selecting just one or two additional cells expressing a particular mixture of antigens.
For example, if the suspected antibody is anti-e, but there are inadequate homozygous cells to exclude anti-Jka on the panel, a cell that is e- Jka+Jkb- can be selected for the purposes of excluding an anti-Jka if non-reactive.
- Note: When antibodies to multiple antigens are suspected (e.g., a large number of cells demonstrate variable strengths of reaction), changing the sensitivity of the testing medium and using inhibiting and enhancing techniques such as polyethylene glycol, proteolytic enzymes and lectins and can be used to distinguish different antigen-reactions from one another.
5: Check the autocontrol to distinguish allo- from auto-antibodies.
One of the cells used during an antibody investigation must be the patient’s own cells (alternatively, an antibody investigation must be accompanied by a direct antiglobulin test).
This is particularly important when all the other cells on a panel react with the patient’s plasma. If the autocontrol agglutinates with the same strength as the other panel cells, this suggests the presence of an autoantibody, whereas a negative autocontrol suggests a collection of multiple alloantibodies or an antibody against a very common (high frequency) antigen.
6: Perform additional tests to confirm alloantibody specificity.
Evidence that an antibody investigation was performed correctly include the absence of the suspected target antigen on the patient’s own cells. For example, a patient with an anti-C would be expected to phenotype as C-negative.
Additional evidence to support the conclusion of the antibody investigation comes from the crossmatch. For example, in a patient with an anti-C, RBCs that are C-negative would not be expected to agglutinate during a serologic crossmatch.
If either patient phenotyping or crossmatching gives unexpectedly positive results, additional investigations are usually required. In addition to an incorrectly performed or interpreted antibody investigation, possible explanations include the presence of an autoantibody, or partial expression of the antigen in question.
7: Report your conclusions.
Your report should include the specificity of the antibody identified, its clinical significance (for example, whether it is known to cause hemolytic disease of the newborn or hemolysis) and the anticipated difficulty in sourcing blood for future transfusions.
The absence of previously identified antibodies, and the possibility that the antibody now reacting may cause hemolysis of recently transfused RBCs (e.g., via a delayed hemolytic transfusion reaction) are also clinically relevant findings to communicate in the report.
